Fetal Reduction
What is Fetal Reduction?
Multiple pregnancies, while naturally occurring, are more common following ovulation induction or assisted reproductive technologies like IVF. During IVF, multiple embryos are often transferred to the uterus to increase the chances of implantation and successful pregnancy. However, transferring more embryos also raises the likelihood of multiple pregnancies.
The higher the number of fetuses, the greater the risk of complications such as premature birth, maternal hypertension, and other serious conditions. To mitigate these risks, fetal reduction is performed to reduce the number of fetuses, ensuring the pregnancy progresses safely.

Why is Fetal Reduction Performed?
When the number of fetuses increases:
- The likelihood of miscarriage in the first trimester rises.
- The risk of premature delivery increases, often resulting in fetuses with underdeveloped organs, particularly the lungs, heart, and brain.
- Premature infants may face lifelong health challenges, including cerebral palsy, intellectual disabilities, and vision or hearing loss.
Fetal reduction minimizes these risks by reducing the number of fetuses to a manageable number, typically one or two. This procedure is also used in cases where one fetus is diagnosed with a severe, untreatable condition.
Risks of Multiple Pregnancies for Mothers
Mothers carrying more than two fetuses are at greater risk of complications, including:

Severe morning sickness and constipation.
Gestational diabetes and hypertension (preeclampsia).
Anemia and placental abruption, a serious condition where the placenta detaches from the uterine wall prematurely.
Frequently Asked Questions FAQ
How is Fetal Reduction Performed?
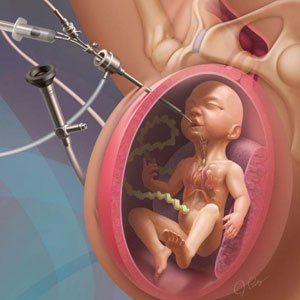
Fetal reduction is typically conducted during the first trimester (around the 12th week of pregnancy) after thorough evaluations to confirm the health of the fetuses. At this stage, the fetuses are enclosed in separate fluid-filled sacs, enabling the doctor to target one without affecting the others.
The procedure is performed under ultrasound guidance and anesthesia to ensure the mother feels no pain. A thin needle is inserted into the uterus, either through the abdominal wall or the vagina. A specialized drug (e.g., potassium chloride) is injected into the targeted sac, stopping the heartbeat of the selected fetus.
In some cases, a technique called radiofrequency ablation is used. This involves using a small device with an electrode to cut off blood flow from the umbilical cord to the selected fetus.
What Happens After Fetal Reduction?
After the procedure, another ultrasound is performed to ensure the remaining fetuses are healthy and to confirm that there are no complications. Although the procedure takes only a few minutes, the mother may need to stay in the hospital for several hours or overnight for observation.
What are the Potential Complications of Fetal Reduction ?
Potential Complications of Fetal Reduction
Most complications are minor, such as:
Pain or bruising at the needle site.
Light vaginal bleeding, typically a few drops of blood.
Rare but serious complications include infection or excessive bleeding. If the mother experiences fever, significant bleeding, or uterine contractions, she should contact her doctor immediately.
Post-Procedure Care for the Mother
To ensure the health of the remaining fetuses, the doctor provides specific recommendations, including:
- A high-calorie, protein-rich diet.
- Taking prescribed medications and nutritional supplements.
- Frequent medical consultations and ultrasounds to monitor the health of both the mother and the fetuses.
Since fetal reduction is often performed following IVF, careful handling of the pregnancy and comprehensive care for the mother are essential. Choosing specialized centers and experienced physicians can significantly improve the outcome of this procedure.
Fetal reduction is a delicate and complex process aimed at safeguarding the health of both the mother and the remaining fetuses, ensuring the best possible outcome for all involved.
